CASE STUDY 4
Author

Professor Dr.med. Jens Tischendorf Chief Physician at the Department of Internal Medicine and Gastroenterology Rhein-Maas Hospital
Würselen, Germany
Patient's Medical History
An endoscopic mucosal resection (EMR) was carried out on the now 83-year-old patient 4 years ago due to Barrett’s epithelium with severe intraepithelial neoplasia. An extended radiofrequency ablation (RFA) was then carried out 3 months later on a remaining long, non-dysplastic Barrett’s segment (C12M13 in accordance with the Prague classification). Further follow-up examinations were not noted by the patient. The patient is now presenting with increasingly dysphagic symptoms.
Endoscopic examination and intervention with dilation
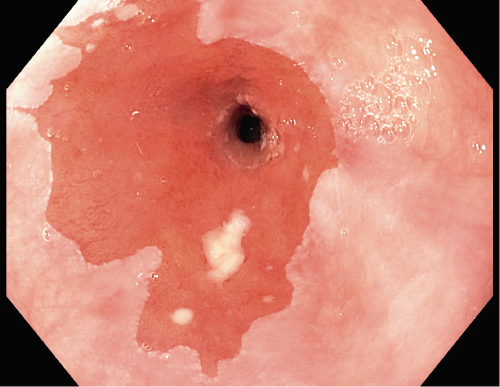
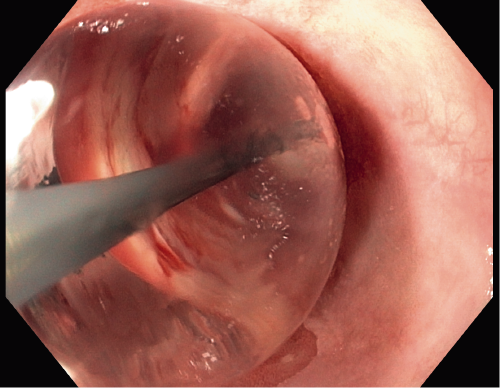
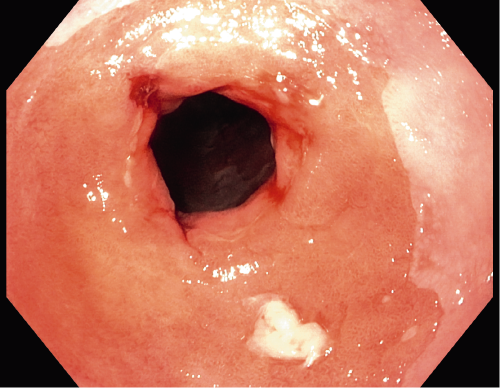
Despite the earlier EMR and RFA, an endoscopic examination showed a long Barrett’s segment (C9M10 in accordance with the Prague classification), in which no dysplasia could be detected by biopsy. A short (5 mm) cicatricial stenosis with a residual lumen of 9 mm (Fig. 1) was found 31 cm aborally correlating with the dysphagic symptoms. The stenosis is localized to the area in which the EMR was carried out 4 years ago. A gradual balloon dilation of the stenosis with the Olympus EZDilate BD-410X-1855 up to a maximum diameter of 18 mm (5.5 atm) was then carried out. Fig. 2 shows the view through the blocked balloon onto the mucosa of the stenosis, which can then be torn in a controlled manner. After dilation the stenosis is significantly wider than before, but there is no indication of perforation or bleeding (Fig. 3).
Procedure and Summary
The patient has already benefited clinically from the first dilation treatment for their cicatricial stenosis. In the event of intrusive residual dysphagia, it would be worth considering dilation to 20 mm.
Despite the wall of the esophagus being thin, gradual dilation carried out with direct visual monitoring offers a safe and effective option for treating stenoses.
- Content Type