VOLUME REDUCTION OF HYPERTROPHIC TURBINATES
In the following chapter, it is demonstrated how to use bipolar radiofrequency-induced thermotherapy (RFITT) to reduce the volume of the hypertrophic inferior turbinates.
01 | Anesthesia and Medications
The turbinates can be treated with RFITT using local anesthesia.
For topical anesthesia, cotton swabs soaked in a two to four percent lidocaine solution are recommended.
Place the swabs around the inferior turbinate for three to five minutes.
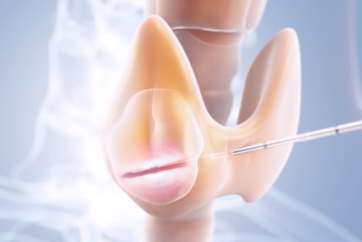
To make sure your patient has no pain during the procedure, it is recommended to inject 2 to 3 ml of a two percent adrenalin-free lidocaine solution into the whole treatment area of the inferior nasal concha [Figure 01a/b].
The injection of lidocaine also increases the volume of the turbinate during the treatment, which reduces the risk of damage to the mucous membrane.
Therefore, do not administer vasoconstrictive substances prior to the procedure, as these would cause a temporary reduction in the volume of the turbinate.
02 | Treatment of the Nasal Turbinates (with RFITT)
Power settings: A power setting of 15 watts (mode: FineRFITT or PureRFITT) is recommended. You can use a higher setting of up to 20 watts to treat smaller turbinates, for instance when you are treating children. The power setting on the control unit determines the extent of coagulation induction. The lower the power setting, the longer the application time and the greater the extent of coagulation. The higher the power setting, the smaller the area of coagulation.
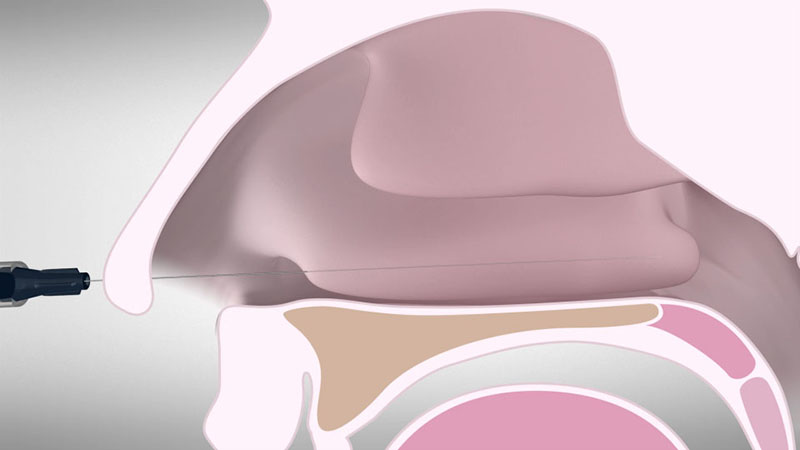
Use the CelonProBreath applicator to treat the hypertrophic turbinate.
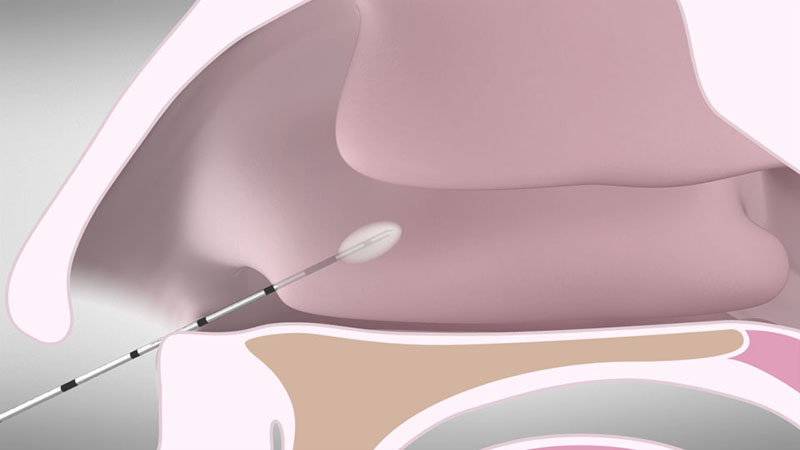
Insert the applicator into the anterior end of the inferior turbinate. In case of a bulky head of the turbinate, the first coagulation should be done in the upper part [Figure 02].
After positioning the applicator, activate the power supply by pressing the foot switch. You can monitor the status of coagulation via the acoustic signal. The power supply is reduced automatically to prevent overdose effects.
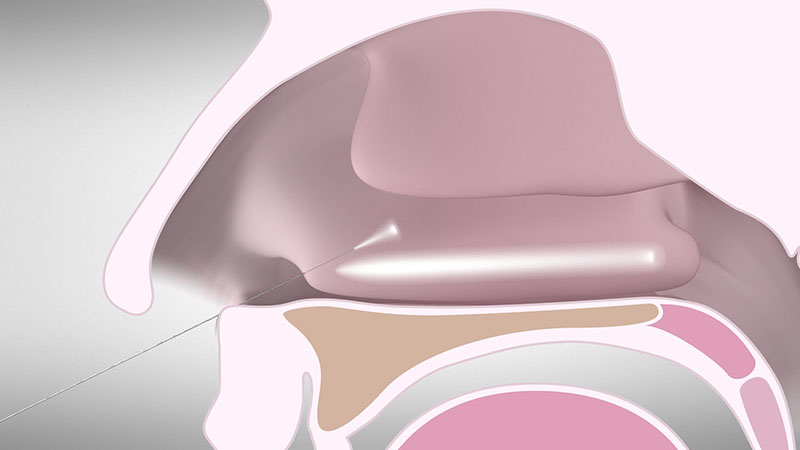
Now reposition the applicator by pulling it out slightly without removing it all the way [Figure 03a]. Insert it posteriorly beneath the mucous membrane [Figure 03b].
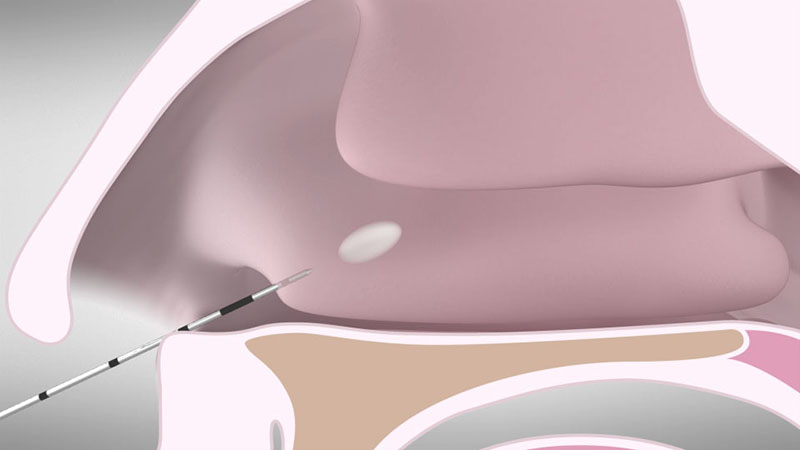
Place the electrode as closely as possible to midway between the bone and mucous membrane.
Depending on the patients’ anatomy, for example if they have a deviated septum, it may be necessary to use additional insertion points near the middle or the posterior end of the turbinate.
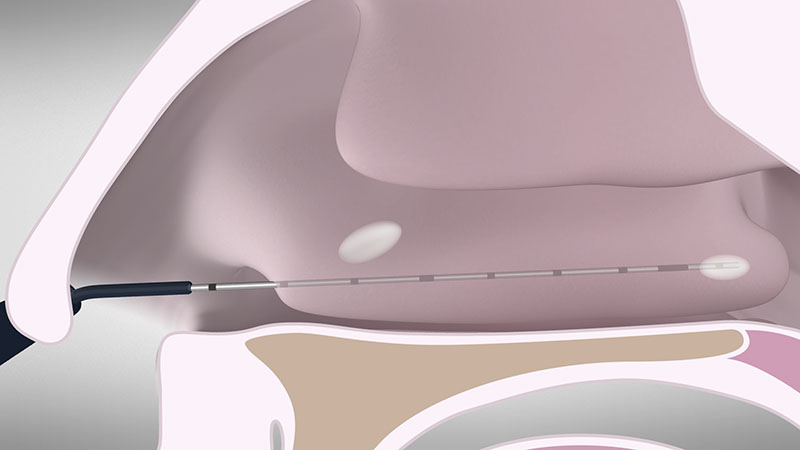
To achieve coagulation along the entire length of turbinate, withdraw the needle repeatedly at around 1.5 cm and reactivate the power control unit [Figure 04 a/b]. You can use the 1 cm markings on the shaft of the applicator as a positioning gauge.
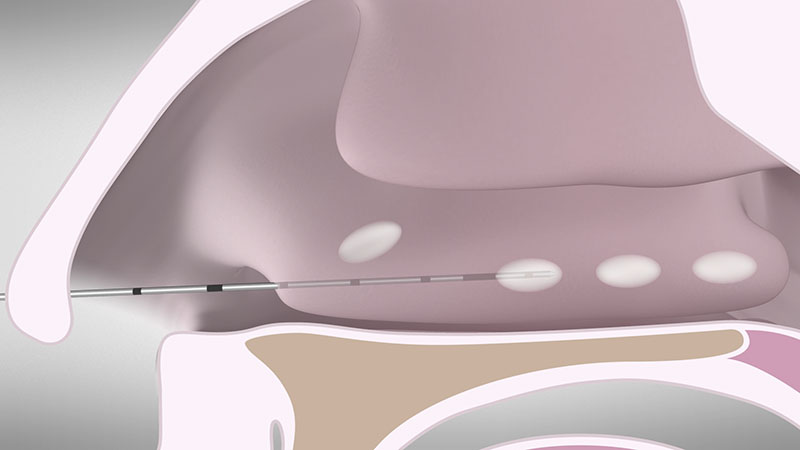
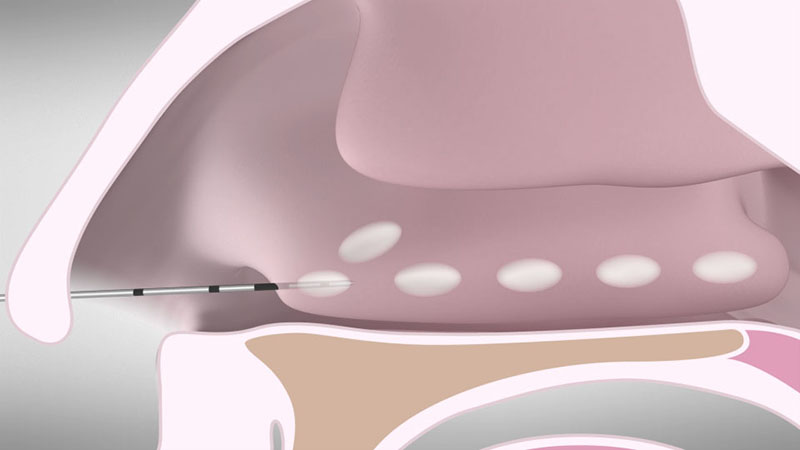
Leaving healthy areas between the lesions will reduce the risk of crusting and improve healing.
Repeat this procedure until the hypertrophic areas of the turbinates have been fully treated.
Note:
If the mucous membrane turns white, interrupt the power output immediately by releasing the foot switch and reposition the applicator. This will avoid injuring the mucous membrane and prevent unnecessary crusting.
03 | Therapeutic Effect
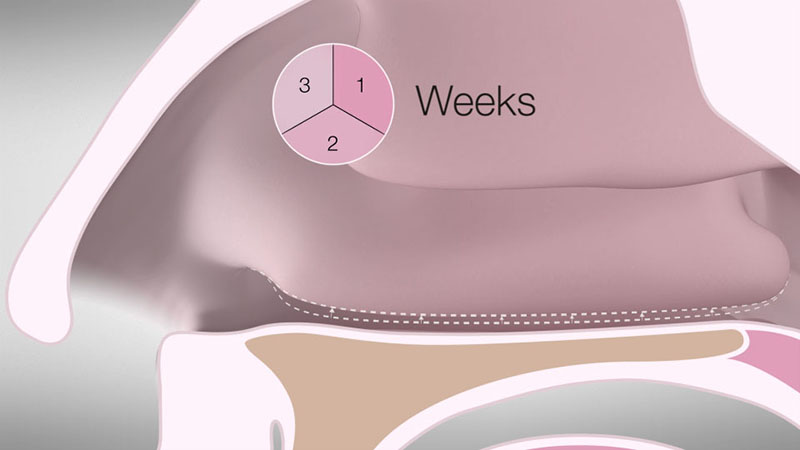
The coagulation achieves a local denaturation of the treated tissue area. Reduction sets in after a few days as a result of scarring and breakdown of the coagulated tissue.
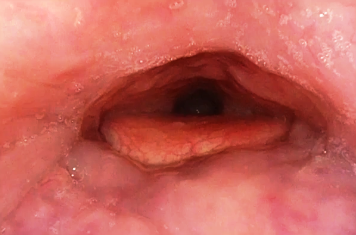
After three weeks, you can expect a visible reduction in volume as a result of scarring and the body’s resorption of the coagulated tissue [Figure 05].
04 | Postoperative Care
Your patients may experience temporary difficulties breathing through their nose until the swelling goes down.
It is recommended to use saline solution and mild nasal ointments postoperatively.
Nasal packing is usually not necessary, since there is normally no bleeding.
Schedule a follow-up visit with your patient the following day in order to check the results and to remove any fibrin formation, which might block the nose.
If your patient’s breathing has not improved after three or four days, it might be necessary to have a second postoperative checkup and cleaning. However, additional CELON treatments of the turbinates are usually unnecessary.
- Content Type