Round-Table Discussion
Benefits of EVIS X1
in the respiratory area
Bronchoscopes serve a dual purpose, acting as instruments to facilitate the use of devices such as biopsy forceps and radial ultrasonic miniature probes for R-EBUS to reach peripheral lesions. Simultaneously, they function as tools for conducting diagnostic imaging through direct lesion observation. The introduction of EVIS X1, a new endoscopy system, has seen improvements in the image enhancement function, a crucial aspect of diagnostic imaging in various medical care areas. However, in the respiratory field, there is only limited documentation of clinical usefullness of the functions of EVIS X1, making the evaluation and collection of additional clinical data about the clinical utility of EVIS X1 necessary. To address this, a round-table discussion was conducted, bringing together expert doctors in respiratory diagnosis and treatment. The discussion focused on the benefits of EVIS X1, including insights from cases experienced at their respective facilities.

2. Evaluating the Clinical Utility of TXI, NBI, and AFI
3. Assessing the Clinical Utility and Future Outlook of RDI
4. Benefits of BAI-MAC and other functions of EVIS X1
5. Assessment of the Clinical Effectiveness of 1200 Series/290 Series Bronchoscopes and their Comparative Analysis
Theme 1. Observation process in bronchoscopies

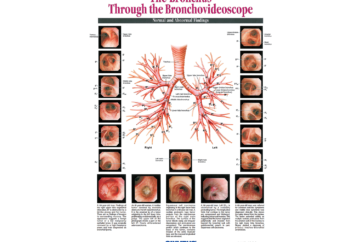
Dr. Himeji: Prior to commencing the discussion on functions of the EVIS X1, I would like to go over the basic observation process in bronchoscopies.
In order to obtain accurate findings in bronchoscopies, it is necessary to observe and evaluate lesions based on the anatomical structure of each bronchial wall layer. The observation process for a bronchoscopy initially involves evaluating the morphological findings regarding the spread of the lesion (localized/non-localized), surface characteristics (color tone), and changes in the tracheal lumen (such as stenotic, dilated, elevated, flat, depressed.) Next, the endoscopic findings in each bronchial wall layer are evaluated in order to determine the disease type classification from the main position of the lesion. In bronchoscopies, the undertaking of diagnoses through this two-step observation process is important.
The anatomical layers of intrapulmonary bronchial wall are classified into four groups termed epithelial layer, subepithelial layer, intramural layer and extramural layer with endoscopic terminology(Fig. 1)1). Additionally, disease types are classified as epithelial, subepithelial, intramural and extramural, according to the respective layer terms.
In evaluation of the endoscopic findings in each layer structure, clarifying the anatomical structures representing these layers (example: elastic fiber bundle of the subepithelial layer) is necessary.
In the course of this observation procedure, the EVIS X1 incorporates not only the established Narrow Band Imaging (NBI) and Auto Fluorescence Imaging (AFI) found in previous models but also introduces advanced image enhancement endoscopy features. These include Texture and Color Enhancement Imaging (TXI), a technology that enhances image quality, and Red Dichromatic Imaging (RDI), a specialized light imaging technique. These additional functionalities hold the potential to be valuable in enhancing the overall utility of the endoscopy process.
In the themes that follow, I am intended to have a discussion on the benefits and separate use of the respective functions.
Theme 2. Evaluating the Clinical Utility of TXI, NBI, and AFI
Dr. Himeji: I will give a brief explanation of TXI, NBI and AFI. TXI is an image processing technology that optimizes the three elements of image, “texture,” “color tone” and “brightness” based on information under white-light imaging (WLI). It can be expected to elevate observation performance by brightening dark areas without causing halation and making it easier to visually confirm slight color tone changes and structural changes on the images. Because NBI improves the visibility of the capillary vessels of the subepithelial layer by utilizing two different wavelengths of narrow-band light (415nm/540nm), it is designed to contribute to lesion screening as well as qualitative and quantitative diagnosis. AFI is a function that highlights neoplastic lesions and normal findings with different color tones based on detected auto fluorescence. AFI aims to improve the detection rate and diagnosis rate particularly in cases where preinvasive lesions or early-stage cancers of the central airway are suspected.
To start, could you please review the areas where you have identified the usefulness of TXI?

Dr. Ishii: By virtue of using TXI when evaluating the epithelium, it has become easier to determine the demarcation of tumors than it is with WLI (Fig. 2), and so in addition to evaluating lesions, conceivably it will also be useful when investigating the presence or absence of surgical indication and the scope of radiotherapy. Previously, I considered the purpose of using TXI to be mainly evaluating epithelial lesions not recognized as masses. However, in a scenario involving a ALK-positive squamous cell carcinoma, the application of TXI allowed for a clear visualization of the mass structure and the trajectory and inflow of blood vessels (Fig. 3). Therefore, I believe it shows benefit in assessing epithelial lesions identified as masses.
At our hospital, for advanced cancer cases, in many instances we perform bronchoscopies for the purpose of establishing a pathological diagnosis. I am hopeful that in the future, it will be possible to detect early-stage cancers by using TXI for screening purposes even in such as bronchial thermoplasty cases. In terms of the challenges going forward, I think there is a need to explore issues such as whether its benefits surpass other image enhancing functions, and whether it also has uses outside the evaluation of epithelial lesions.
Dr. Morikawa: My impression is that by using TXI the structure of each layer, mainly the position of blood vessels and membranous portion, becomes even more recognizable. Therefore, I think it will be possible to fully capitalize on its strengths even in situations where peripheral lesions are observed, not just central lesions. Additionally, I experienced a case in which using TXI made it easier to evaluate the excision range when removing a tumor (Fig. 4).
Dr. Nakai: In a situation where lung cancer in the upper right lobe was resected, the utilization of TXI during the observation of main bronchial stenosis post-bronchoplasty allowed me to identify alterations in the epithelium that were not discernible with WLI. Consequently, it was diagnosed as stenosis caused by fibrotic changes, not recurrent cancer. As a result, I was able to clearly determine that it was not a recurrence of the cancer, but respiratory stenosis resulting from a fibrotic change (Fig. 5). Moreover, there was an instance where I could accurately determine the biopsy site and the scope of radiotherapy for a skip lesion within the respiratory tract, which was not entirely confirmable with WLI. This precision was achievable due to the improved visibility provided by TXI. In this case, I find TXI to be highly beneficial as it enables a more intricate observation compared to WLI, whether it involves a normal lesion or a non-malignant tumor. Going forward, as actual clinical data on TXI is accumulated, TXI can be expected to prove useful even in detecting epithelial lesions.
Dr. Himeji: According to your insights, it seems that TXI has proven advantageous in observing various aspects, including the identification of lesion locations, surface characteristics, lesion demarcations, background epithelium, and alterations in blood vessels and existing structures. Additionally, you highlighted the potential of TXI, extending to the diagnosis of peripheral lesions and the assessment of biopsy sites, radiotherapy scope, and the extent of tumor excision. Next, could you please go over the areas where you have found NBI useful?
Dr. Morikawa: In a case of sarcoidosis, despite the challenge of visually confirming blood vessels in the membranous sections using WLI, clear observation became feasible through the use of NBI (Fig. 6). I believe NBI holds the potential to be particularly effective in scenarios where there is a need to observe subepithelial capillaries.
Dr. Himeji: As you two have indicated, conceivably NBI is useful when determining the border of a lesion or obtaining findings from subepithelial blood vessels.
Next, could you please go over cases pertaining to the benefits of AFI?
Dr. Morikawa: In a case of EGFR gene Exon 21 lung cancer in which polypoid lesions were recognized in the right bronchus intermedius, I used AFI in order to visually confim if the lesion infiltrates the surrounding tissue or not (Fig. 8). In a case where there are multiple endobronchial metastases, confirming all small lesions is extremely difficult, but I feel AFI is useful for making it possible to get a grasp of the extent and number of lesions at a certain level.
Dr. Himeji: It seems you have highlighted the usefulness of AFI in acquiring insights into lesion qualities, such as the overall background epithelium and color tone, akin to conventional models. Could you elaborate on the key points regarding the individual utilization of these functions and their future prospects?
Dr. Morikawa: When there was no TXI option, we were taught that we should observe the shape and trajectory of blood vessels mainly using NBI. However, because TXI has made it possible to delineate as far as the blood vessels of the subepithelial layer, and because the color tone of obtained images is also emphasized under TXI, I believe that in the future there is a possibility NBI will be replaced by TXI for observing the course of blood vessels.
Dr. Nakai: In my perspective, the observations we’ve traditionally made with AFI could potentially be approached differently using TXI. An advantage of TXI might be its capability to conduct examinations with color tones closely resembling WLI, which could facilitate seamless exploration of peripheral lung lesions. This implies that, following the initiation of an examination with TXI and blood flow confirmation, detailed observations of suspected lesion areas using NBI may eliminate the need to switch to the AFI scope, potentially reducing the patient’s burden.
Dr. Himeji: For instance, in cases of squamous cell carcinoma, abnormalities can be observed in the epithelial layer. However, in some instances, distinguishing adenocarcinoma through the observation and biopsy of the subepithelial layer and below proves challenging. In such scenarios, the proficient utilization of each function for distinct purposes to achieve accurate findings becomes crucial. It appears evident that each of you is adopting a strategy where TXI is primarily employed for screening and assessing morphological characteristics. Additional functions beyond TXI are incorporated when scrutinizing capillary areas or determining lesion demarcations in greater detail.
Theme 3. Assessing the Clinical Utility and Future Outlook of RDI
Dr. Himeji: I would like to move on to a discussion about the clinical utility of RDI. Blood vessels etc. that are observed as red with WLI are visually confirmed as orange and amber with RDI, so RDI enhances contrast to blood vessels, consequently contributing to improve the visibility of bleeding spots and deep blood vessels. Could you please go over the areas where you have found RDI useful?
Dr. Nakai: When I judge whether there is bleeding from a coagra in a scenario involving the identification of a left main bronchial tumor, the visual confirmation of the absence of bleeding from the epithelium through RDI observation played a crucial role in ensuring the safe execution of tumor excision and stent placement (Fig. 9). This suggests that RDI is designed to improve the visibility of deep blood vessels, to enable tumors to be removed while avoiding blood vessels. In addition, at our hospital, there are cases in which we perform full-thickness biopsies when performing thoracoscopic surgery under local anesthesia, and there is a possibility RDI will be useful in cases such as this also.
Dr. Morikawa: It is conceivable that RDI could prove useful in situations involving the evaluation of cases where there is a significant increase of vascularization, and sporadic thick blood vessels, in the subepithelial layer. In fact, I have used RDI for the purpose of avoiding vascular damage in situations where I was selecting tumor biopsy locations. When collecting tissue samples, I employ RDI to enhance the visibility of blood vessels. Deep blood vessels appear red in RDI Modes 1 and 2, while they appear green in RDI Mode 3 (Fig. 10). This enhancement in visibility, accentuating blood vessels, proves quite useful. Furthermore, RDI enables color-coding of the deep portion and the surface layer, serving as a valuable foundation for assessing the depth of blood vessels during biopsies. Consequently, it has the potential to contribute to safer biopsy procedures with a diminished risk of bleeding.
Alternatively, RDI has the potential not only to make it possible to visually confirm single blood vessels, but also to enable the confirmation of blood flow distribution through coloring. For example, in a case of small-cell lung cancer in the right upper lobe, when a tumor is observed under RDI, necrotic tissue is rendered white, and locations where there is a degree of abundant blood flow are rendered in reddish amber in Mode 1 and green in Mode 3. With RDI, I think it is possible to obtain information indicating the area containing viable cells, which is not visualized with NBI (Fig. 11).
As a personal outlook, I hope to pathologically verify the differences in coloring resulting from deep portions/shallow portions, differences in vascular diameter and so on that arise in RDI observation.
Dr. Ishii: I think using RDI makes it possible to observe biopsy locations more clearly and makes it easier to effectively suction blood immediately following biopsies. In a case of suspected primary ciliary dyskinesia, I used RDI when performing cryobiopsies (Fig. 12). In order to investigate ciliary dyskinesia, I biopsied the 8-9, 9-10 bifurcations. It is important not to perform the biopsy in the same site for the purpose of obtaining a large number of cilia. In the process of using RDI, the visibility of the biopsy locations was enhanced more than under WLI, so I experienced the benefits of employing RDI in selecting biopsy locations. Moreover, during bronchial thermoplasties, especially in cases where bleeding is more probable than in normal scenarios, I find RDI to be beneficial for conducting hemostasis procedures and assessing blood vessels before surgery.
Dr. Himeji: In summary of your collective insights, it seems that beyond RDI’s confirmed utility in identifying bleeding spots, for which a consensus has been established, you have also highlighted its role in “ensuring safety.” This includes its value as a foundation for determining biopsy locations with a minimized risk of bleeding. Moreover, the prospect of RDI being employed to verify biopsy location positions post-biopsy and in thoracoscopies, prompts the hope for further exploration in this direction.
Theme 4. Benefits of BAI-MAC and other functions in EVIS X1
Dr. Himeji: Let us consider the benefits of other functions of EVIS X1 (Table 1). BAI-MAC (Brightness Adjustment Imaging with Maintenance of Contrast), which is incorporated in EVIS X1, is a function that enhances the visibility of the mid to far distant point without prolonging halation by selectively elevating the brightness solely at the dim distant point, while retaining the brightness of the near point. Conceivably, this could contribute to enhanced observation performance, mainly during screening tests.
What were your impressions of using the BAI-MAC function?
Dr. Ishii: For me personally, I always have BAI-MAC switched on during my procedures. In situations requiring a peripheral approach with the EBUS-GS method, upon comparing the use of BAI-MAC versus its absence, the deeper bifurcation points became more clearly delineated with BAI-MAC activated (Fig. 13). Additionally, with regard to the image quality as well, I have the impression that images are more vivid with BAI-MAC on. Accordingly, it is conceivable that using BAI-MAC can lead to improved ability to inspect deeper bifurcations.
Dr. Morikawa: I am in a similar situation, where I basically perform procedures with BAI-MAC constantly on. In fact, my impression is that by using BAI-MAC, it has become possible to clearly observe one bronchus deeper than the other.
Dr. Nakai: I had a case involving a peripheral lung lesion slated for biopsy from the left B4b based on a virtual bronchoscopy, I activated BAI-MAC just before inserting an ultrasonic miniature probe for R-EBUS. This allowed for the observation of a tumor infiltrating a peripheral bronchus of the left B4a, prompting a modification in the approach route. This meant that I was able to reach the lesion easily (Fig. 14). In fact, conceivably BAI-MAC has the advantage of enabling a larger amount of information to be provided to bronchoscopists without any drawback. I think a benefit of BAI-MAC is that using it enables to visually confirm deep bronchi at a glance, so I routinely have the function switched on.
Dr. Himeji: There appears to be agreement among all of you regarding benefits of BAI-MAC. Other than BAI-MAC, are there any other functions in the EVIS X1 that you view as particularly useful?
Dr. Ishii: EVIS X1 is equipped with “Disconnect scope” function which allows us to disconnect scopes without powering down the video system center, CV-1500. I frequently switch scopes during procedures, so I feel this function is useful.
Dr. Morikawa: The CV-1500, the video system center for the EVIS X1, employs a touch panel operation rather than buttons, which is a point I feel is useful. I have impression that the touch panel enhances the operability, even if we cover the touch panel part with a vinyl sheet at our hospital from an infection prevention perspective.
Theme 5. Assessment of the Clinical Effectiveness of 1200 Series/290 Series Bronchoscopes and their Comparative Analysis
Dr. Himeji: The BF-H1200/BF-1TH1200, which are equipped with high-sensitivity CMOS image sensors, have been launched as EVIS X1 series’ scopes (Table 2). With BF-H1200, the instrument channel inner diameter is larger than its predecessor, the BF-H290 (the channel inner diameters of BF-H1200 and BF-H290 are 2.2 mm and 2.0 mm, respectively), even while having a distal end outer diameter of 4.9 mm (the BF-H290’s distal end outer diameter is 6.0 mm), which can be expected to lead to enhanced performance in forceps procedures. Additionally, with BF-1TH1200, although the distal end outer diameter is smaller than its predecessor, the BF-1TQ290 (the outer diameters of BF-1TH1200 and BF-1TQ290 are 5.8mm and 5.9mm, respectively), the instrument channel inner diameter has been maintained at 3.0 mm, so it can be expected to deliver suction performance unchanged from its predecessor.
Could you present cases in which you have used the various scopes, and then discuss their clinical utility?
Dr. Ishii: I feel the BF-1TH1200 is useful in terms of enhancing the image quality because more distinct rendering of the color tones of lumens and the respiratory epithelium, and the course of blood vessels is possible, compared to the BF-1TQ290 (Fig. 15). Additionally, I get the impression that there is not much difference between the BF-H1200 and its BF-P290 predecessor in terms of the range of bronchi that are insertable with the bronchoscopes. When selecting a deeper branch, the BF-P290 has a finer distal end outer diameter than the BF-H1200 and so is superior in terms of the depth it can reach, but I feel the BF-H1200 can also be inserted to quite a depth. Because the BF-H1200 has an instrument channel inner diameter that is 0.2 mm thicker compared to the BF-P290, its cryoprobe insertion performance is enhanced, and so wherever possible I use the BF-H1200 for cryo-biopsies of upper lobe bronchi.
In Bronchoalveolar Lavage (BAL) procedures, the BF-H1200 allows us to insert into one level deeper bronchi and to observe lumens and bubbling more distinctly than its predecessor, the BF-1TQ290. The retrieval rates for BAL carried out at our hospital are around 40-60% with the BF-1TQ290 and around 70% with the BF-H1200, which hints at the usefulness of BAL using the BF-H1200. Because solid wedging of the scope is important for BAL, I think the BF-H1200 is useful in this regard.
Dr. Morikawa: In comparing the BF-1TH1200 and BF-6C260 when observing tracheal squamous cell carcinoma, with the BF-1TH1200 both images under WLI and NBI were clear, and in focus across all areas in the monitor view (Fig. 16). I think the BF-1TH1200 offers higher resolution and brightness when observing in middle to long distance views.
Dr. Nakai: In some cases, it can also take time to get lesions into focus with the BF-P290. On the other hand, in my view, even for doctors who are not yet used to bronchoscopy, the BF-H1200 will make it easy to focus accurately. The fact that the three-dimensionality of the epithelial layer and the detailed structure of blood vessels can be clearly observed in this model with a single touch is useful. Moreover, the broad field of view allows clear observation even from positions distant from stenosis, alleviating stress on bronchoscopist. The substantial volume of information within the angle of view adds to these advantages. Additionally, the BF-H1200 can be inserted into the peripheral bronchus while treating the central one, making it an exceptionally convenient and user-friendly scope.
Dr. Himeji: After listening to all of you, I got the feeling that the BF-H1200/BF-1TH1200 can be used broadly for everything from observation through to intervention. With regard to the smaller distal end diameter and the larger instrument channel inner diameter of BF-H1200, do you ever feel the BF-H1200 is useful when performing cryobiopsies?
Dr. Ishii: Concerning the suction capability, the BF-H1200 will be slightly inferior compared to the BF-1TH1200. However, the BF-H1200 can be inserted as far as the deeper part of the bronchi, and I use it with peace of mind when performing cryobiopsies also.
Dr. Nakai: When treating masses in the respiratory tract, I am able to complete the treatment using the BF-H1200 alone, without switching the scope. I feel the BF-H1200 is convenient because it can be inserted to depper into the bronchi, and it also maintains sufficient suction performance. In particular, it offers good compatibility with a 1.7-mm cryoprobe, and the scope’s operability remains favorable after the probe is attached. If you set a short freezing period the procedure can be completed with little bleeding, so the treatment can be continued with little stress.
Dr. Himeji: Dr. Morikawa, you have a wealth of experience with interventions. In your case, what scope do you choose for cryobiopsies?
Dr. Morikawa: My first choice when performing cryobiopsies is the BF-1TQ290. However, up to now I have also experienced a large number of cases where the stenosis has been strong, and it has not been possible to insert a scope with a 5.9-mm distal end outer diameter. With the BF-H1200, I am able to observe in higher image quality compared to the BF-1TQ290, so going forward I intend to actively use the BF-H1200 in cases where the stenosis is strong.
Dr. Himeji: This suggests that as a result of using the EVIS X1 and its compatible scopes, the BF-H1200/BF-1TH1200, the image quality is further enhanced compared to their predecessors and so there is a possibility bronchoscopists will be able to obtain more beneficial findings. However, when it comes to bronchoscopies, it is possible to maximize the utility of the discussed functions in this round-table discussion by obtaining findings while carefully considering the implications of the observation items based on the anatomical structure of the bronchi. Additionally, it will be important not to stop with obtaining high-quality findings alone, but to carry out day-to-day medical care while being conscious of what sorts of benefits will be delivered to patients thanks to those findings.
Everyone, thank you very much for your time today.
References: 1) Kiyoshima M, et al. The Journal of the Japan Society for Respiratory Endoscopy. 2018; 40: 401-413.

Any content or information (“Content”) presented herein is illustrative in nature and does not guarantee or represent specific information, outcomes, or results. Olympus Medical Systems Corp. and its parents, subsidiaries, affiliates, directors, officers, employees, agents, and representatives (collectively “Olympus”) does not represent to or warrant the accuracy or applicability of the Content. Under no circumstances shall Olympus be liable for any costs, expenses, losses, claims, liabilities, or other damages (whether direct, indirect, special, incidental, consequential, or otherwise) that may arise from, or be incurred in connection with, the Content or any use thereof.
- Content Type


![[Fig. 1] Anatomical layers of intrapulmonary bronchial wall and their endoscopic terminology for disease type classifications](https://www.olympusprofed.com/wp-content/uploads/2024/05/fig.11.png)
![[Fig. 2] Comparison of images under WLI and TXI in a case of squamous cell carcinoma (Dr. Ishii) (a) Observed under WLI](https://www.olympusprofed.com/wp-content/uploads/2024/05/Fig2a.png)
![[Fig. 2] Comparison of images under WLI and TXI in a case of squamous cell carcinoma (Dr. Ishii) (b) Observed under TXI](https://www.olympusprofed.com/wp-content/uploads/2024/05/Fig2b.png)
![[Fig. 3] Comparison of images under WLI and TXI in a case of ALK-positive squamous cell carcinoma (Dr. Ishii) (a) Observed under WLI](https://www.olympusprofed.com/wp-content/uploads/2024/05/Fig3a.png)
![[Fig. 3] Comparison of images under WLI and TXI in a case of ALK-positive squamous cell carcinoma (Dr. Ishii) (b) Observed under TXI](https://www.olympusprofed.com/wp-content/uploads/2024/05/Fig3b.png)
![[Fig. 4] Comparison of images under WLI and TXI in a case in which small-cell lung cancer recurred in a patient with a history of triple lung cancer (Dr. Morikawa) (a) Observed under WLI](https://www.olympusprofed.com/wp-content/uploads/2024/05/Fig4a.png)
![[Fig. 4] Comparison of images under WLI and TXI in a case in which small-cell lung cancer recurred in a patient with a history of triple lung cancer (Dr. Morikawa) (b) Observed under TXI](https://www.olympusprofed.com/wp-content/uploads/2024/05/Fig4b.png)
![[Fig. 5] Comparison of images under WLI and TXI in a case in which main bronchial stenosis developed following an upper right lobe lung cancer resection and bronchoplasty (a) Observed under WLI](https://www.olympusprofed.com/wp-content/uploads/2024/05/Fig5a.png)
![[Fig. 5] Comparison of images under WLI and TXI in a case in which main bronchial stenosis developed following an upper right lobe lung cancer resection and bronchoplasty (b) Observed under TXI](https://www.olympusprofed.com/wp-content/uploads/2024/05/Fig5b.png)
![[Fig. 6] Comparison of images under WLI and NBI in a case of sarcoidosis (Dr. Morikawa) (a) Observed under WLI](https://www.olympusprofed.com/wp-content/uploads/2024/05/Fig6a.png)
![[Fig. 6] Comparison of images under WLI and NBI in a case of sarcoidosis (Dr. Morikawa) (b) Observed under NBI](https://www.olympusprofed.com/wp-content/uploads/2024/05/Fig6b.png)
![[Fig. 7] Comparison of images under WLI and NBI in a case in which a left main bronchial tumor was recognized (Dr. Nakai) (a) Observed under WLI](https://www.olympusprofed.com/wp-content/uploads/2024/05/Fig7a.png)
![[Fig. 7] Comparison of images under WLI and NBI in a case in which a left main bronchial tumor was recognized (Dr. Nakai) (b) Observed under NBI](https://www.olympusprofed.com/wp-content/uploads/2024/05/Fig7b.png)
![[Fig. 8] Comparison of images under WLI and AFI in a case of EGFR gene lung cancer in which polypoid lesions were recognized in the right bronchus intermedius (Dr. Morikawa) (a) Observed under WLI](https://www.olympusprofed.com/wp-content/uploads/2024/05/Fig8a.png)
![[Fig. 8] Comparison of images under WLI and AFI in a case of EGFR gene lung cancer in which polypoid lesions were recognized in the right bronchus intermedius (Dr. Morikawa) (b) Observed under AFI](https://www.olympusprofed.com/wp-content/uploads/2024/05/Fig8b.png)
![[Fig. 9]Comparison of images under TXI and RDI in a case in which a coagulative left main bronchial tumor was recognized (Dr. Nakai) (a) Observed under TXI](https://www.olympusprofed.com/wp-content/uploads/2024/05/Fig9a.png)
![[Fig. 9]Comparison of images under TXI and RDI in a case in which a coagulative left main bronchial tumor was recognized (Dr. Nakai) (b) Observed under RDI](https://www.olympusprofed.com/wp-content/uploads/2024/05/Fig9b.png)
![[Fig. 10] Use of RDI for selection of the biopsy location (Dr. Morikawa) (a) Observed under WLI](https://www.olympusprofed.com/wp-content/uploads/2024/05/Fig10a.png)
![[Fig. 10] Use of RDI for selection of the biopsy location (Dr. Morikawa) (b) Observed under RDI (Mode 2)](https://www.olympusprofed.com/wp-content/uploads/2024/05/Fig10b.png)
![[Fig. 10] Use of RDI for selection of the biopsy location (Dr. Morikawa) (c) Observed under RDI (Mode 3)](https://www.olympusprofed.com/wp-content/uploads/2024/05/Fig10c.png)
![[Fig. 11] Comparison of images under WLI, NBI and RDI in a case of small-cell lung cancer in the right upper lobe (Dr. Morikawa) (a) Observed under WLI](https://www.olympusprofed.com/wp-content/uploads/2024/05/Fig11a.png)
![[Fig. 11] Comparison of images under WLI, NBI and RDI in a case of small-cell lung cancer in the right upper lobe (Dr. Morikawa) (b) Observed under NBI](https://www.olympusprofed.com/wp-content/uploads/2024/05/Fig11b.png)
![[Fig. 11] Comparison of images under WLI, NBI and RDI in a case of small-cell lung cancer in the right upper lobe (Dr. Morikawa) (c) Observed under RDI (Mode 1)](https://www.olympusprofed.com/wp-content/uploads/2024/05/Fig11c.png)
![[Fig. 11] Comparison of images under WLI, NBI and RDI in a case of small-cell lung cancer in the right upper lobe (Dr. Morikawa) (d) Observed under RDI (Mode 3)](https://www.olympusprofed.com/wp-content/uploads/2024/05/Fig11d.png)
![[Fig. 12] Comparison of images under WLI and RDI following biopsies in a case of suspected primary dyskinetic cilia syndrome (Dr. Ishii) (a) Observed under WLI](https://www.olympusprofed.com/wp-content/uploads/2024/05/Fig12a.png)
![[Fig. 12] Comparison of images under WLI and RDI following biopsies in a case of suspected primary dyskinetic cilia syndrome (Dr. Ishii) (b) Observed under RDI (Mode 1)](https://www.olympusprofed.com/wp-content/uploads/2024/05/Fig12b.png)
![[Fig. 12] Comparison of images under WLI and RDI following biopsies in a case of suspected primary dyskinetic cilia syndrome (Dr. Ishii) (c) Observed under RDI (Mode 2)](https://www.olympusprofed.com/wp-content/uploads/2024/05/Fig12c.png)
![[Fig. 12] Comparison of images under WLI and RDI following biopsies in a case of suspected primary dyskinetic cilia syndrome (Dr. Ishii) (d) Observed under RDI (Mode 3)](https://www.olympusprofed.com/wp-content/uploads/2024/05/Fig12d.png)
![[Table 1] Functions in the EVIS X1 at a glance](https://www.olympusprofed.com/wp-content/uploads/2024/05/table1.png)
![[Fig. 13] Comparison of images under WLI with BAI-MAC switched on and off in a case in which it was necessary to approach the periphery with the endobronchial ultrasonography using a guide sheath (EBUS-GS) method (Dr. Ishii) (a) Observed with BAI-MAC off](https://www.olympusprofed.com/wp-content/uploads/2024/05/Fig13a.png)
![[Fig. 13] Comparison of images under WLI with BAI-MAC switched on and off in a case in which it was necessary to approach the periphery with the endobronchial ultrasonography using a guide sheath (EBUS-GS) method (Dr. Ishii) (b) Observed with BAI-MAC on](https://www.olympusprofed.com/wp-content/uploads/2024/05/Fig13b.png)
![[Fig. 14] Comparison of images under WLI with BAI-MAC switched on and off in a case involving a peripheral lung lesion that was scheduled to be biopsied from the left B4b with reference to a virtual endoscopy (Dr. Nakai) (a) Observed with BAI-MAC off](https://www.olympusprofed.com/wp-content/uploads/2024/05/Fig14a.png)
![[Fig. 14] Comparison of images under WLI with BAI-MAC switched on and off in a case involving a peripheral lung lesion that was scheduled to be biopsied from the left B4b with reference to a virtual endoscopy (Dr. Nakai) (b) Observed with BAI-MAC on](https://www.olympusprofed.com/wp-content/uploads/2024/05/Fig14b.png)
![[Table 2] Comparative table of 1200 series/290 series bronchoscopes](https://www.olympusprofed.com/wp-content/uploads/2024/05/table2.png)
![[Fig. 15] Comparison of images under WLI using the BF-1TQ290 and the BF-1TH1200 when observing upper left lobe B1+2 and B3 (Dr. Ishii) (a) Observed using the BF-1TQ290](https://www.olympusprofed.com/wp-content/uploads/2024/05/Fig15a.png)
![[Fig. 15] Comparison of images under WLI using the BF-1TQ290 and the BF-1TH1200 when observing upper left lobe B1+2 and B3 (Dr. Ishii) (b) Observed using the BF-1TH1200](https://www.olympusprofed.com/wp-content/uploads/2024/05/Fig15b.png)
![[Fig. 16] Comparison of images under NBI using the BF-1TH1200 and the BF-6C260 in a case of squamous cell carcinoma (Dr. Morikawa) (a) Observed using the BF-1TH1200](https://www.olympusprofed.com/wp-content/uploads/2024/05/Fig16a.png)
![[Fig. 16] Comparison of images under NBI using the BF-1TH1200 and the BF-6C260 in a case of squamous cell carcinoma (Dr. Morikawa) (b) Observed using the BF-6C260](https://www.olympusprofed.com/wp-content/uploads/2024/05/Fig16b.png)