Imaging Techniques Observation of the gallbladder
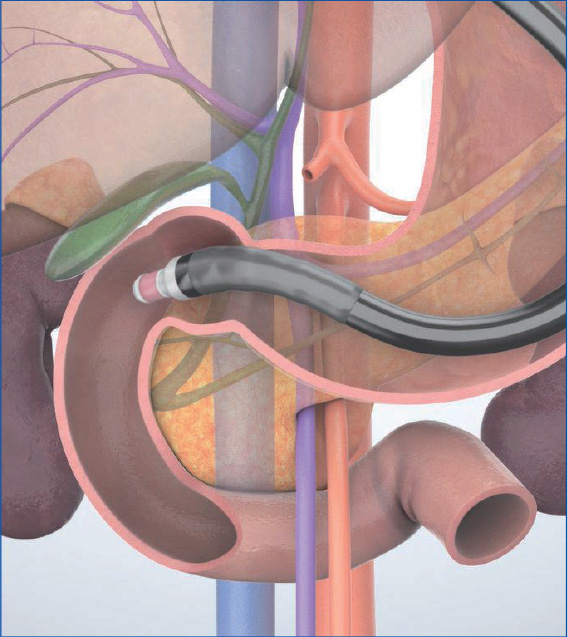
When scanning in the ‘short-scope’ position in the descending part of the duodenum and begin to pull the scope, you can continuously image the distal bile duct all the way to the cystic duct and gallbladder.’ When observing the gallbladder, inflate the balloon to prevent the scope from slipping out of the duodenum and back into the stomach. Then angulate the scope tip to the left or the right as necessary until the entire gallbladder is visualized in the long axis. In some cases, it may be difficult to observe the entire gallbladder in the “short-scope” position. If so, take the “long-scope” position from the gastric antrum or the duodenal bulb to make it easier to observe the gallbladder.
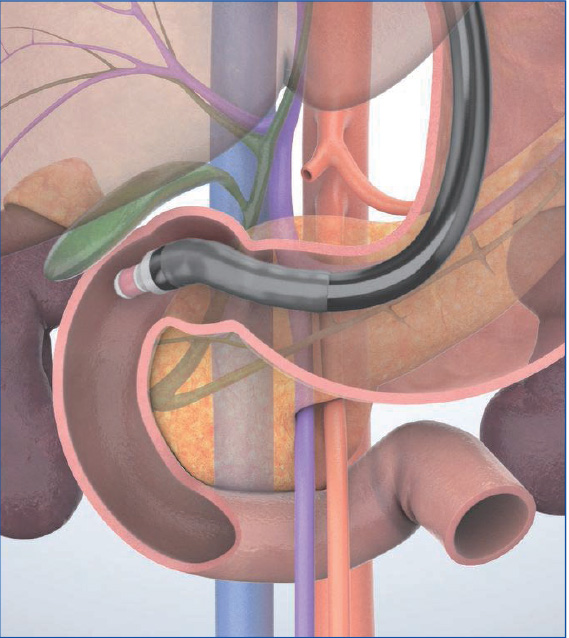
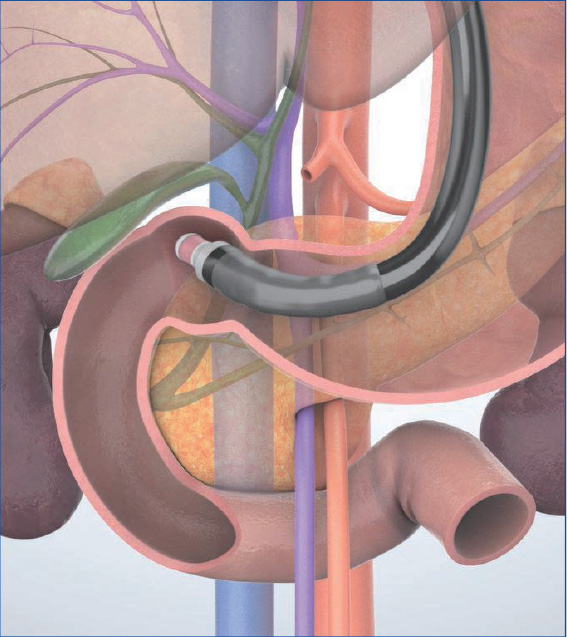
“Short-scope” position
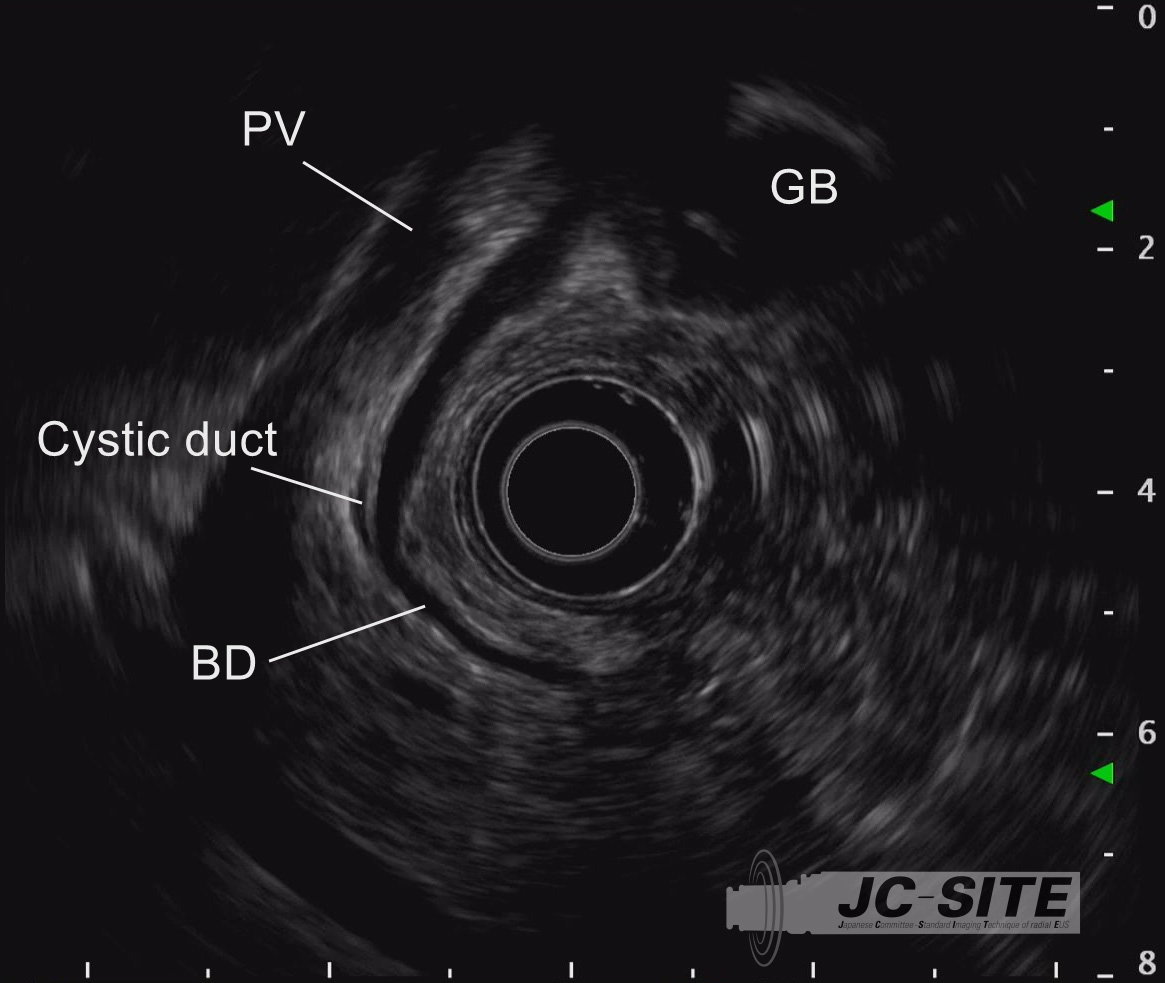
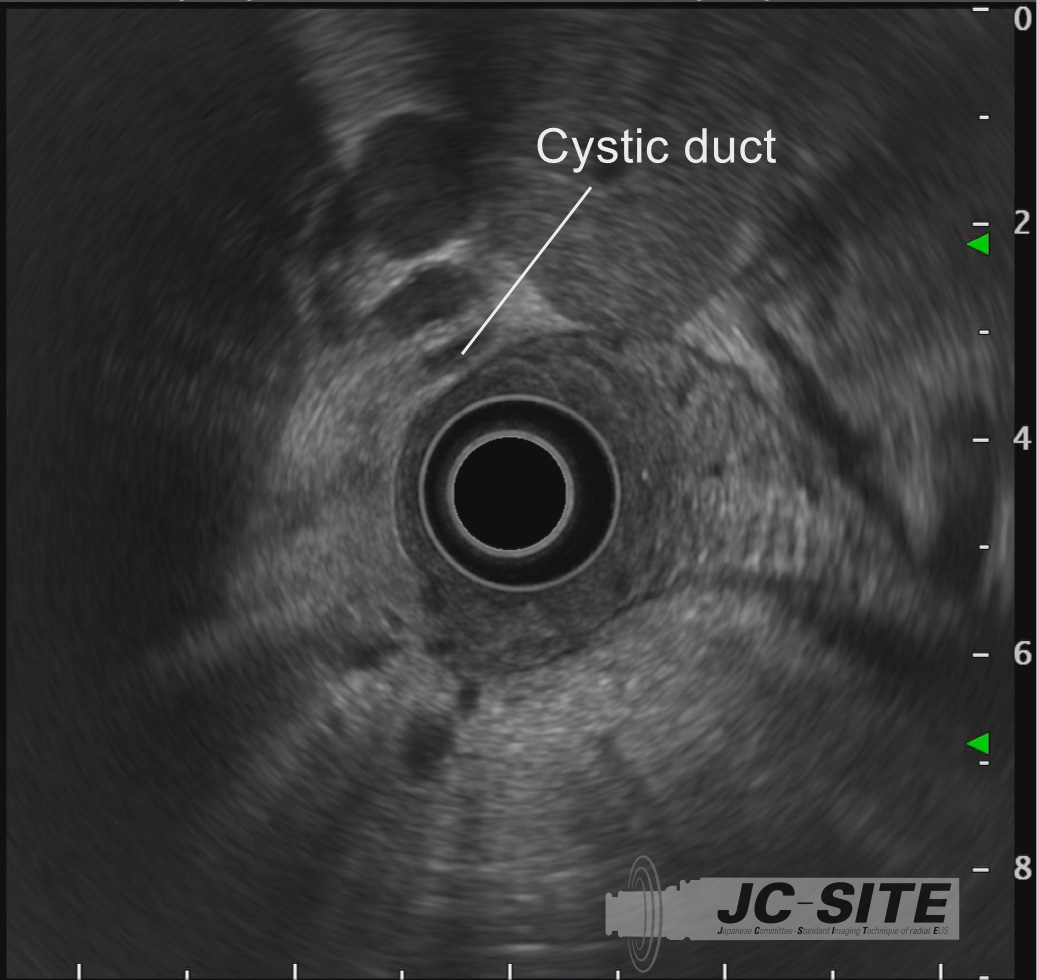
STEP 1
First image the bile duct in the long axis by scanning it from the descending part of the duodenum. Then pull the scope little by little, while rotating it counterclockwise so as not to miss the bile duct. Observe the cystic duct confluence while doing so.
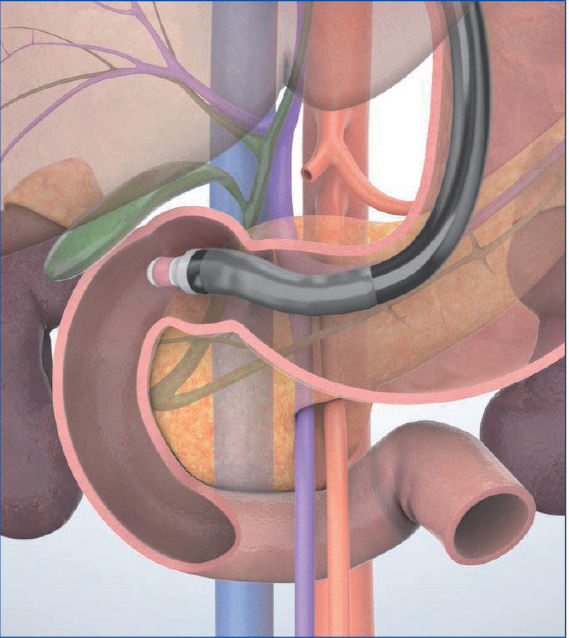
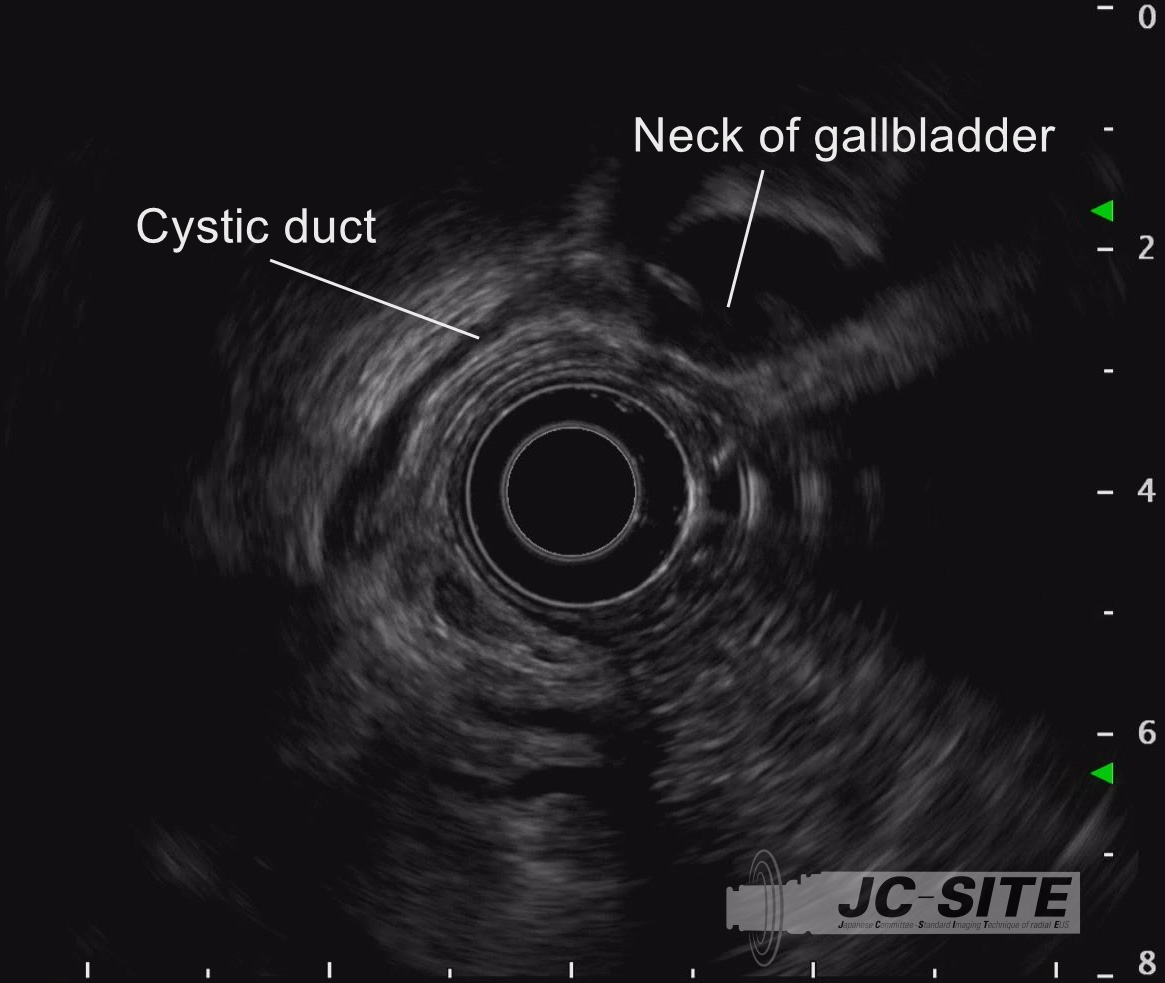
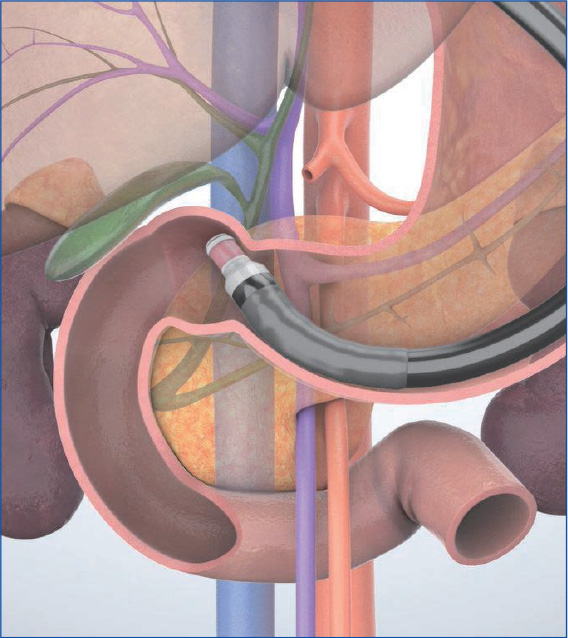
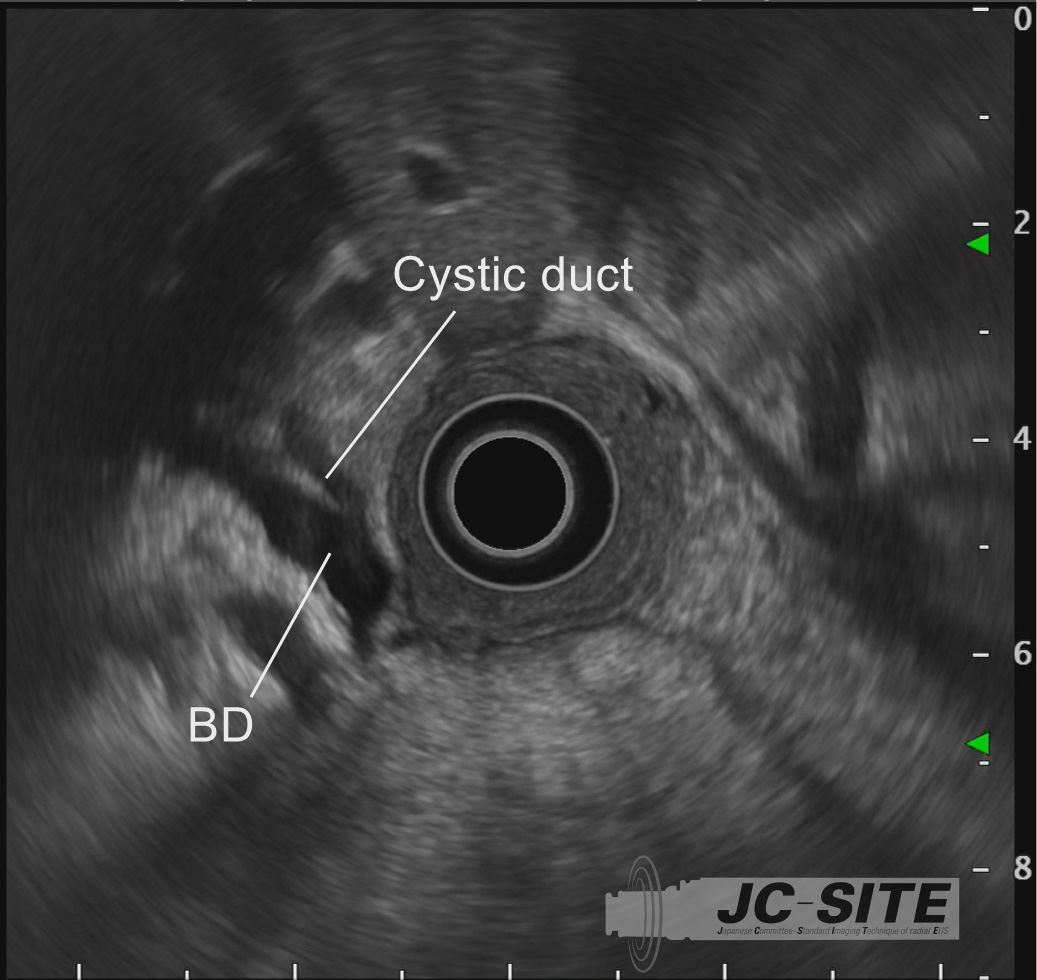
STEP 2
Follow the cystic duct and observe it continuously as far as the neck of the gallbladder.
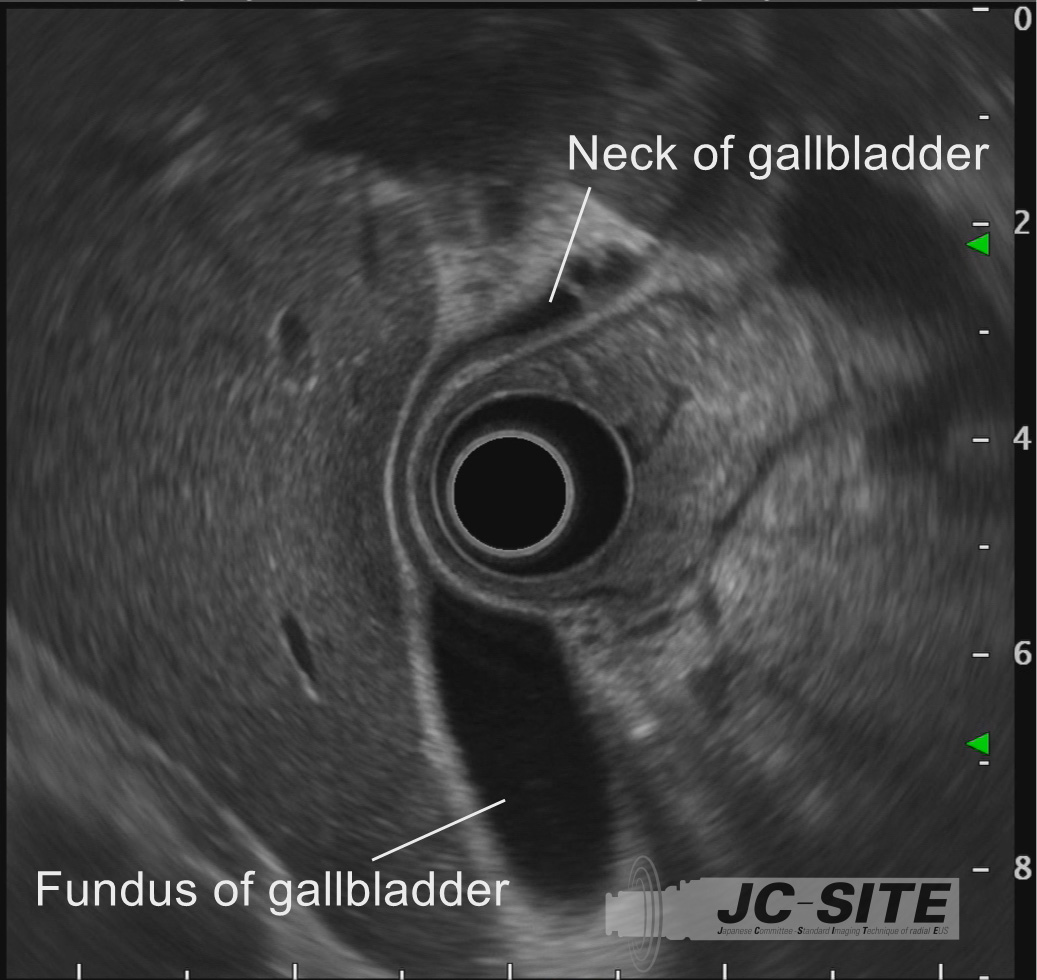
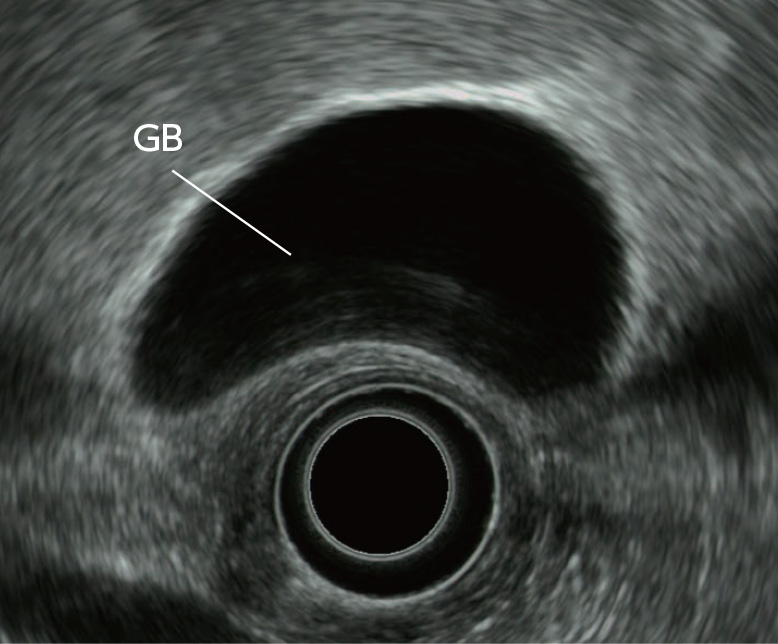
STEP 3
After observing the neck of the gallbladder, angulate the scope tip to the left or right as necessary to observe the entire gallbladder. Usually, the neck of the gallbladder is displayed on the left of the screen, and the fundus on the right.
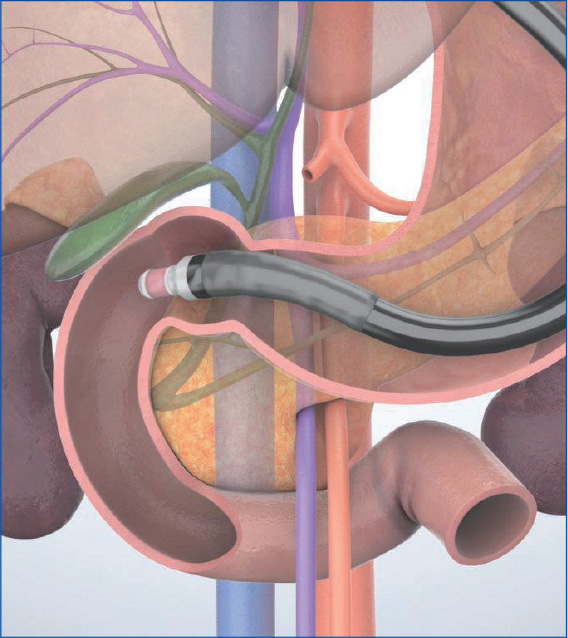
“Long-scope” position
STEP 1
When the scope is inserted into the duodenal bulb in the “long-scope” position, the scope tip points to the proximal side. Hence, the neck of the gallbladder is displayed on the right of the screen, and the fundus on the left.
STEP 2
From here, advance the scope while angulating the scope tip upward and rotating the insertion tube clockwise to observe the neck of the gallbladder and the cystic duct.
STEP 3
Continue to advance the scope to the point where the cystic duct joins the bile duct. Here you can observe the bile duct running towards the papilla.

Layer structures of the gallbladder, bile duct, and papilla and diagnosis of tumor invasion depth and extension
The wall of the gallbladder is imaged as a 3-layer or 2-layer structure in EUS (Fig. a). The 3-layer structure is interpreted as follows: Starting from the luminal side of the gallbladder, the high-echo layer (1st layer) corresponds to the interface echo and the mucosa (m). The low-echo layer (2nd layer) corresponds to the proper muscle layer (mp) and the superficial area of the subserosal layer (ss). The high-eco layer (3rd layer) corresponds to the deeper ss and the serosa (s). The 2-layer structure is interpreted as follows: The inner low-echo layer contains the m, mp, and superficial ss while the outer high-echo layer corresponds to deeper ss and s.
Diagnosis of the invasion depth of a tumorous lesion is relatively easy if the lesion is a Type Ip pedunculated tumor. If the tumor is sessile, diagnose the invasion depth while monitoring the continuity of the gallbladder wall structure in the area where the tumor is attached. If continuity is maintained in the outer high-echo layer, it means that part of T1 (invasion into m and mp) or T2 (ss or invasion into the connective tissues around the muscle layer in the fundus of the gallbladder) invasion is present. If the outer layer is ruptured, it is possible to diagnose the lesion as T2 or more advanced.
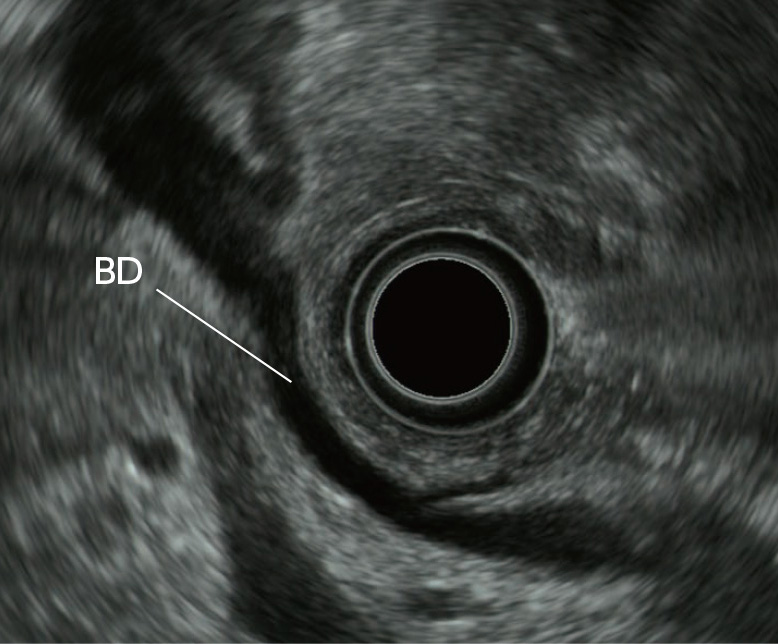
In EUS, the wall of the bile duct is imaged as a 2-layer structure with an inner low-echo layer and outer high-echo layer (Fig. b). The inner low-echo layer contains the mucosa (m), fibromuscular layer (fm), and superficial area of subserosa (ss). The outer high-echo layer corresponds to the deep area of ss. If the bile duct shows a localized change, malignancy should be suspected. If there is diffuse thickening of the bile duct, the tumor can be assumed to be benign. However, differential diagnosis between benign and malignant is often difficult in EUS.
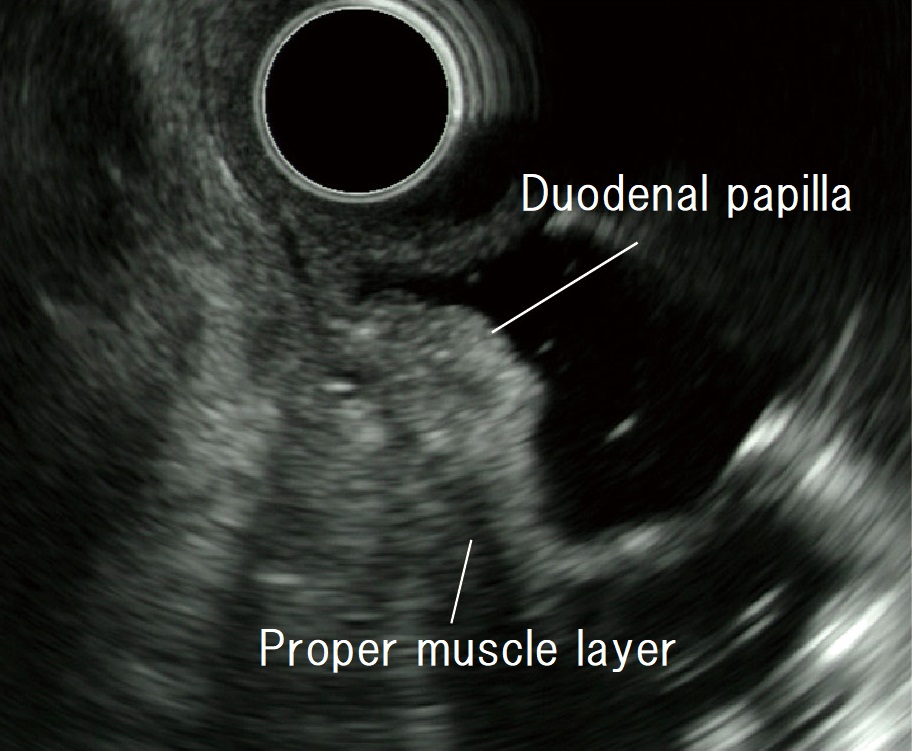
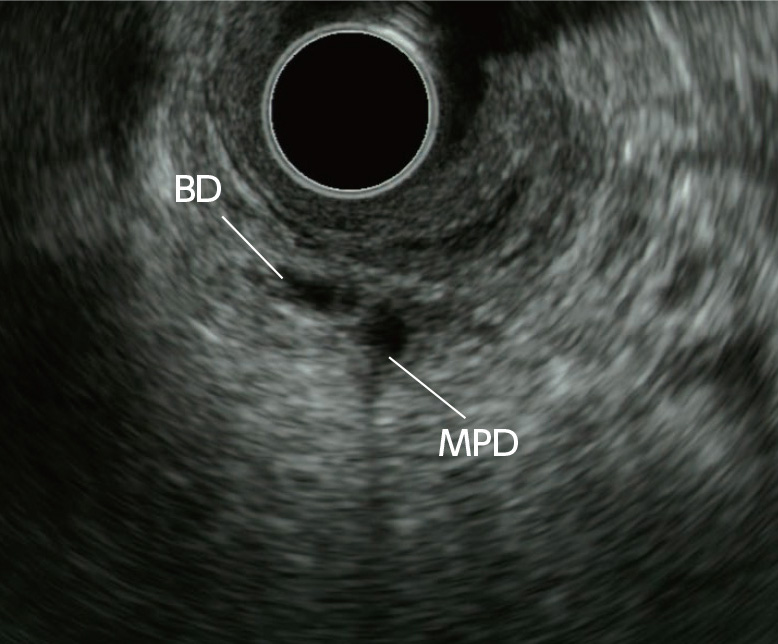
Regarding the papilla, scan the proper muscle layer of the duodenum, common channel, pancreatic duct, bile duct, and pancreatic parenchyma using EUS (Figs. c, d). If the lesion is tumorous, compare the tumor with the scanned images in order to stage the tumor. In EUS, the presence of duodenal invasion (Du-invasion) and pancreatic invasion (Panc-invasion) is determined by referring to the proper muscle layer of the duodenum. Imaging the sphincter of Oddi is generally considered difficult when the papilla is normal.
- Content Type